Resonance Health offers patients magnetic resonance imaging (MRI) based alternatives to invasive medical procedures. Patients need no longer undergo the painful, time consuming process of liver biopsy for the diagnosis, monitoring and treatment planning for iron overload or fatty liver disease.
Resonance Health offers the following services:
- FerriScan® – MRI Measurement of Liver Iron Concentration for patients with overload disorders (offered with or without a Cardiac T2* measurement for a more complete overview of iron loading)
- HepaFat-Scan® – MRI Measurement of Liver Fat for patients with fatty liver disease.
- Bone Marrow R2-MRI – MRI based solution for assessing iron levels in the bone marrow.
- FerriSmart® – Fully-automated A.I. MRI Measurement of Liver Iron Concentration for patients with overload disorders
HepaFat-Scan® Information for Patients
HepaFat-Scan is a magnetic resonance imaging (MRI)-based technology for the non-invasive measurement of liver fat. It provides a reliable measure of volume percentage of liver fat for screening, diagnosis, treatment planning and monitoring of patients in a variety of clinical settings.
What Does HepaFat-Scan Offer You?
- A non-invasive – safe and painless alternative to liver biopsy
- An accurate result
- A faster alternative, resulting in reduced anxiety for patients by providing a reduction in testing and result waiting times.
- A test which can be used repeatedly, allowing for increased quality of life through more efficient testing and treatment programs.
Potential Clinical Applications
Gastroenterology and Hepatology Applications
- Initial workup for Non Alcoholic Fatty Liver Disease (NAFLD) diagnosis and for patient education and counselling.
- Liver fat analysis on patients already being screened or monitored for fibrosis or cirrhosis.
Surgical Applications
- Fatty liver assessment prior to liver surgery, due to increased complications with the presence of liver fat
- Screening for suitability of living donors for liver transplants by assisting in determining the viability of the liver
- Pre and post operative analysis of bariatric patients to track clinical outcomes.
Applications by Primary Care Physicians
- HepaFat-Scan may be useful to screen patients prior to prescribing known hepatotoxic medications.
- Monitoring of patients undergoing an intervention (e.g. limiting alcohol consumption or weight loss)
- Monitoring of patients prescribed medications known to induce steatosis
Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD) is a name that is given to a range of liver disorders associated with the presence of too much fat in the liver. Steatosis is a mild form of fatty liver. In some patients with steatosis, inflammation of the liver may occur with resultant hepatitis called non-alcoholic steatohepatitis (NASH).
Risk Factors
Risk factors for NAFLD include obesity, diabetes, insulin resistance and hyperlipidemia.
How Common is NAFLD:
NAFLD is considered the most common liver disease in the western world affecting 20-30% of the population, rising to 70-90% of the obese population and approximately 50% of the diabetic population. In 2012 nearly 70% of US adults were overweight, with 35% of adults in the obese category. In the UK, according to the 2012 Health Survey for England, approximately one quarter of adults are obese.
NAFLD is estimated to occur in approximately 30% of adults in the United States. NASH is present in 2-5% of individuals. With the current obesity epidemic, these percentages continue to increase.
Patients with NAFLD, especially those with mild steatosis, rarely have symptoms. Patients may present in one of three ways:
- A mild increase in liver size may be noted on physical exam, warranting further testing.
- An elevation of liver enzymes may be noted on routine laboratory testing.
- The presence of fat in the liver may be an incidental finding on an imaging study such as an ultrasound or CT scan which is obtained for an unrelated reason.
The amount of liver fat can now be quantified with HepaFat-Scan. Early detection of steatosis (liver fat) facilitates the early diagnosis and intervention before liver damage may become irreversible.
NAFLD Linked to Diabetes and Liver Cancer:
Steatosis has also been linked to reduced effectiveness of antiviral treatments and has been implicated in the development of type 2 diabetes. Non-alcoholic fatty liver disease (NAFLD) is an independent predictor of type 2 diabetes according to a study presented at the European Association for the Study of the Liver International Liver Congress 2014.
In a retrospective study (3074 subjects) conducted in Japan, people with NAFLD had nearly three times the risk of developing diabetes than people without the condition, according to Hajime Yamazaki, MD, of Teine Keijinkai Hospital in Sapporo, Japan, and colleagues. At the > 10 year follow up, he found that 16.1% of the 728 patients with NAFLD had developed type 2 diabetes, versus only 3.1% of the remaining 2346 NAFLD negative patients. The odds ratio for the NAFLD association was 6.05 (P<0.001). A multivariate analysis adjusted for confounders such as age, sex, BMI, family history of diabetes and dyslipidemia and the odds ratio remained significant at 2.82 (P<0.001). Moreover, improvements in NAFLD reduced the risk of diabetes over about an 11-year follow-up, Yamazaki told an oral session. Ultrasound follow up analysis at >10 years showed that 110 of the 728 subjects with NAFLD had an improvement in their NAFLD and the incidence of type 2 diabetes in this group was 6.4% vs 17.8% in the group with no improvement in NAFLD. Dr Yamazaki stated that “The clinical message is that it is important to reduce fatty liver to prevent diabetes”.
Recent research suggests a strong association between hepatic steatosis and hepatocellular carcinoma (HCC) in the absence of cirrhosis, indicating that steatosis may be a causative factor for HCC.
A French study (5671 subjects) also presented at the European Association for the Study of the Liver International Liver Congress 2014 found that NAFLD is an independent predictor of carotid atherosclerosis. C-IMT, carotid plaques and Framingham risk scores were all significantly higher in the 1871 subjects with NAFLD vs the 3800 without the disease. All were independent of age, sex, BMI, hypertension and tobacco use. Dr Raluca Pais, MD, PhD from of Pitié-Salpêtrière Hospital in Paris stated that “Patients at risk for CVD should probably be screened for fatty liver, regardless of the transaminase levels, because NAFLD is an independent predictor of cardiovascular risk, beyond traditional risk factors like metabolic syndrome”.
As the evidence against fatty liver mounts, researchers and clinicians are embarking on studies that require the measurement of liver fat content so that it can be correlated with health risks and other clinical parameters such as age and overall weight gain or loss. Biopsy is often unacceptable for such studies and hence non-invasive methods are required. HepaFat-Scan® provides such a solution.
FerriScan® Information for Patients
FerriScan is a magnetic resonance imaging (MRI)-based technology for the non-invasive measurement of liver iron concentration. The test is designed to assist in the diagnosis and treatment planning for patients with iron loading disorders (commonly referred to as "iron overload" conditions).
Perth patient, John Falconer, who was diagnosed with haemochromatosis when he was 75, says that FerriScan was a great alternative to an invasive liver biopsy.
"I have had three MRI's now and would recommend FerriScan to anyone. The results are quick and give a very informative report and accurate reading of your iron liver concentration. The scans have helped monitor and plan my treatment. I certainly wouldn't have wanted to have a liver biopsy."
– John Falconer.
What Does FerriScan Offer You?
- A non-invasive – safe and painless alternative to biopsy.
- An accurate result, allowing for early disease detection which can prevent long term damage.
- Large image area which decreases sampling error and provides a more reliable and meaningful result than liver biopsy.
- A faster alternative, resulting in reduced anxiety for patients by providing a reduction in testing and result waiting times.
- A test which can be used repeatedly, allowing for increased quality of life through more efficient testing and treatment programs.
"I was a nurse and yet I'd never heard of haemochromatosis or iron overload. I thought if I hadn't heard of it, then there were probably many in the medical community who hadn't either and people were most likely walking around with iron overload like me and remaining undetected for years. The FerriScan was quick and painless and is an excellent alternative to liver biopsy for patients who want to find out their exact level of iron loading. The Haemochromatosis Society is working with the providers of FerriScan, Resonance Health, to promote awareness of iron overload and improve health outcomes for people affected by this disease."
– Margaret Rankin; Patron and Past President of Haemochromatosis Australia.
What is iron overload?
Iron overload is the accumulation of excess iron in the body. People who receive multiple blood transfusions in the course of treatment for certain diseases are at particular risk of iron overload as the body has no natural mechanism for excreting iron. One unit of transfused red cells delivers approximately 250mg of iron to the body. People with thalassaemia, sickle cell anaemia, Diamond Blackfan anaemia and myelodysplastic syndrome may receive regular blood transfusions, resulting in a need to monitor total body iron, and where appropriate, to remove it through chelation therapy. More recently, iron overload is becoming increasing recognised as a complication in cancer survivors who received multiple blood transfusions as part of their cancer therapy. To read more about the application of FerriScan in this setting please refer here: Iron Overload in Cancer Survivors.
Iron overload can also be caused by excessive absorption of iron from the diet, as occurs in the hereditary disease haemochromatosis.
Clinicians managing these conditions require a complete picture of a patient’s body iron stores to inform their decisions on treatment options.
Accurate monitoring of liver iron concentration (LIC) provides essential information in the prevention of iron-related complications and premature death in iron overloaded patients.
Modell B. Br Med Bull. 1976;32:270
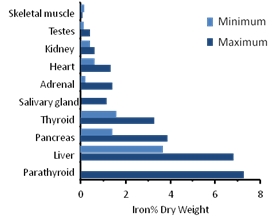
This graph shows the organs in which iron deposition occurs when there is excess iron in the bloodstream.
The liver is the primary site of iron storage in the body.
Why Monitor Liver Iron?
Deposits of iron in tissues cause organ damage, and accumulation occurs primarily in the liver. Once the iron-binding capacity of the liver has been exceeded, deposition occurs in other organs, such as the heart. This causes a greater risk of cardiac complications and premature death.
Therefore, monitoring of liver iron concentration provides an early warning of potential cardiac iron loading and its attendant health implications.
Update on Imaging: Detection of Iron in Liver in Heart – Webcast and Powerpoint presentation by Professor Tim St Pierre – from European Society of Haematology website: 'The Curriculum in Iron Metabolism and Related Disorders'
Why Monitor Cardiac Iron?
The deposition of cardiac iron has profound implications for patient health and indicates that urgent measures must be taken to reduce body iron loading.
An analysis of both liver and cardiac iron therefore enables clinicians to get a more complete picture of body iron loading, to appraise the immediate health risks to the patient and inform their decisions on treatment options.
Why Choose Resonance Health?
Our methods only require patients to have a quick, easy and painless MRI scan. There is no risk from radiation and the process does not require any contrast agents.
Our products are quality assured and regulatory cleared in USA, Europe and Australia; assuring we provide accurate and reliable results.
If you suspect you may have an iron overload condition or fatty liver disease, please see your clinician for a referral to one of our approved Radiology Centres.